Injection technique tips for palatal anesthesia

For beginning practitioners, developing an effective local anesthesia injection technique is an excellent way to help grow your practice. This can be done without the inconvenience of buffering solutions and avoiding the expense of products such as The Wand.

Topical Anesthetic Gel

Use a quality topical anesthetic gel; avoid cheap, less potent, low-viscosity generic products. If the product has a runny consistency, patients will be more likely to swallow it and feel as if they are choking. One of the excellent products available is Premier’s Topicale. It has a pleasant taste to most patients and it’s both viscous and potent, so only a minimal amount is necessary.

Short Needle Injections

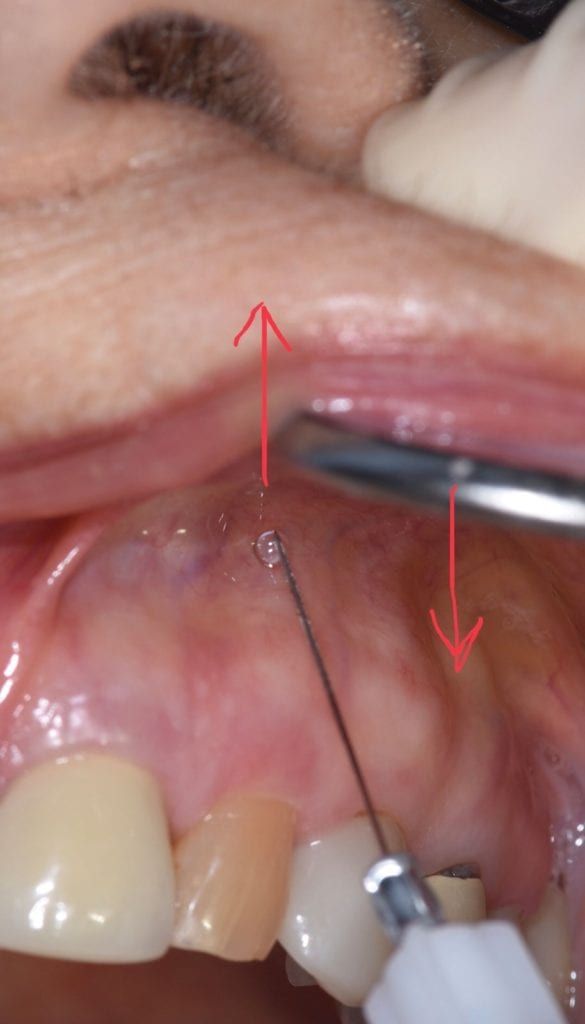
I use septocaine 4% epi 1:100,000 with a 30-gauge short needle for all maxillary injections, unless use of epinephrine is contraindicated for that patient. Here is a key: Pause for a moment just before the needle penetrates the mucosa. For the maxillary arch, gently grasp the lip, stabilized with a mirror, as pictured, then quickly but carefully advance the needle into the mucosa while simultaneously pulling the lip and soft tissue into the needle. This is a two-handed technique. The sensory movement of the tissue blocks much of the pain transmission down the neural pathway. Take your time, allowing 45–60 seconds to administer while gently moving the tissue back and forth. Comment to your patient while doing so about doing it gently, taking time to make it more comfortable, and ask them if they’re doing OK. Afterward, I’ll ask patients, “Now, that wasn’t too rough, was it?” It’s nice to hear them make a positive comment afterward, and it may be helpful to the patient to verbalize that it was better than they anticipated.

20-degree Angle for Anesthetic Needle
I prefer to put about a 20-degree angle on my anesthetic needles. In dental school, we were told to never bend an anesthetic needle, but modern, heat-treatable stainless steel needles are malleable to an extent. I’ve angled my needles for every injection over the past 36 years of my career and have never had one break. (Only bend a needle once, however!) A bent needle allows me to keep my elbows more at my side and prevents me from leaning more often out of my ergonomic position. Anything to help with posture, because it adds up by the end of the day.

Pain Modulation
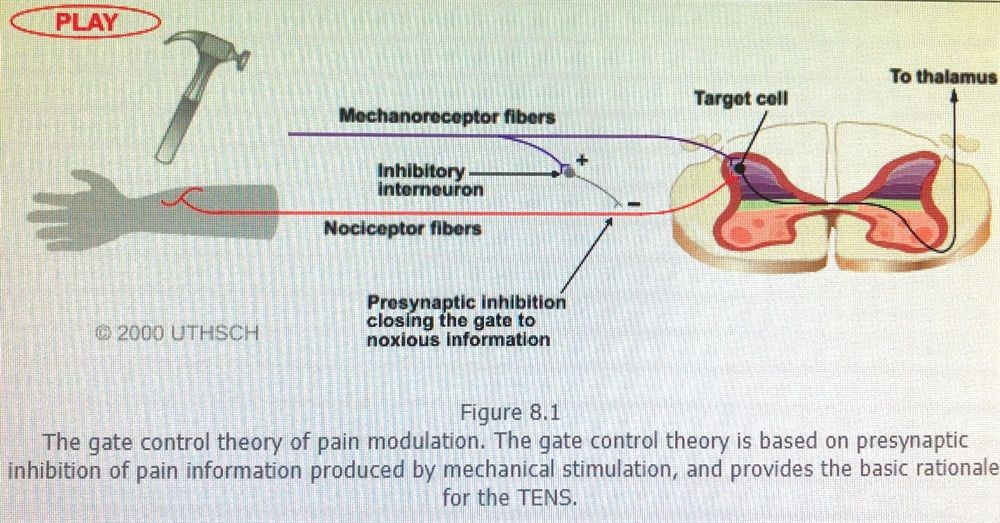
There is a theory as to why moving this tissue during the injection procedure is effective. The large sensory fibers that carry the cutaneous sensory input have collaterals that activate inhibitory interneurons. These inhibit pain transmission carried by the pain fibers. This non-noxious input “closes the gate” to noxious input.

IAN Block Procedure

For the inferior alveolar block, I use a 27-gauge long needle with 2% lidocaine epi 1:100,000 unless contraindicated. For every IAN block procedure, I give two injections and (surprisingly) have not heard a complaint about this yet. This should really improve your success rate. The first will be in a high position and the second lower, as pictured, in the pterygomandibular depression lateral to the raphe. This is helpful because the position where the inferior alveolar nerve enters the mandibular canal in the ramus varies from patient to patient.
Again, there is that momentary pause before simultaneously advancing the cheek/buccal mucosa grasped between your thumb (in the coronoid notch) and opposing finger and quickly advancing the needle into the mucosa. Gently feel for the needle bump into the medial surface of the ramus, slightly anterior to where you estimate the mandibular canal to be. Withdraw slightly, then advance the needle posteriorly to the appropriate depth, aspirate, then express the anesthetic. Have the patient open and close a few times after the first injection before giving the second. Again, use the same slow administration, soft tissue movement and calm reassurance to the patient while administering.

Anesthetic Warming Dispenser

Use an anesthetic warming dispenser. They’re only about $75 and it will last for years. Having the anesthetic solution close to body temperature will make a big difference in patient comfort. Turn the anesthetic warmers off at the end of each workday. It takes about 30 minutes in the morning for the carpules to reach the desired temperature of 105 degrees Fahrenheit, and leaving them on 24/7 can eventually affect the efficacy of the anesthetic if stored there for too long. Speaking of efficacy—again, avoid a generic local anesthetic and use a name-brand product! In my experience, there is definitely a difference in the effectiveness. You are not saving money by using a cheaper product here.

Never Inject Directly on the Palate

Never give an injection directly on the palate. After administering the infiltration anesthetic as previously described, you should be able to inject into the mesial and distal buccal mucosa in a minute or less. Inject a second time into the buccal interproximal areas.

Palatal Soft-tissue Injection

Start the palatal soft-tissue injection in the palatal interproximal area. I count to 15 using very light pressure, then to 15 using moderate pressure, then to about 10 or longer using stronger pressure. Visualize the tissue blanching. Advance the needle to the periphery of the blanched tissue, as seen in Fig. 10. The patient will not feel the next injection if the needle penetrates blanched tissue. Generally, in four minutes or less you can anesthetize any maxillary tooth with minimal or no discomfort.
Dr. John A. Batlle III graduated from the University of Florida College of Dentistry in 1983, then served as an assistant dental director and senior dentist with the Florida Department of Corrections. He concurrently served in the U.S. Navy Reserve for 26 years, retiring as a captain. In the final decade of his military career, Batlle was attached to the Marines and provided dental support for deployments around the world. For the past 11 years, Batlle has been in solo private practice at Southwest Family Dentistry in Lake City, Florida. He holds a courtesy clinical assistant professor position at the U.F. College of Dentistry, and has provided faculty support on several of the U.F. dental student mission trips to Central and South America.

